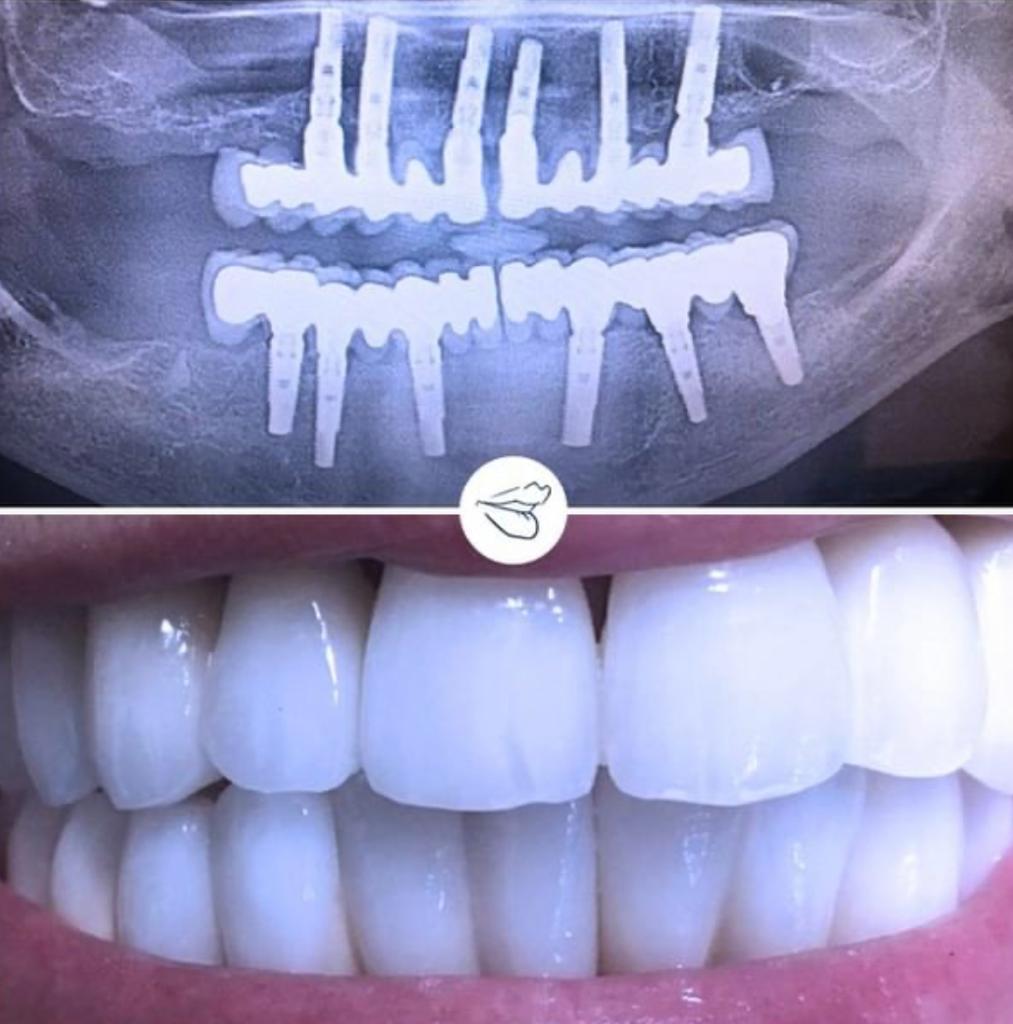
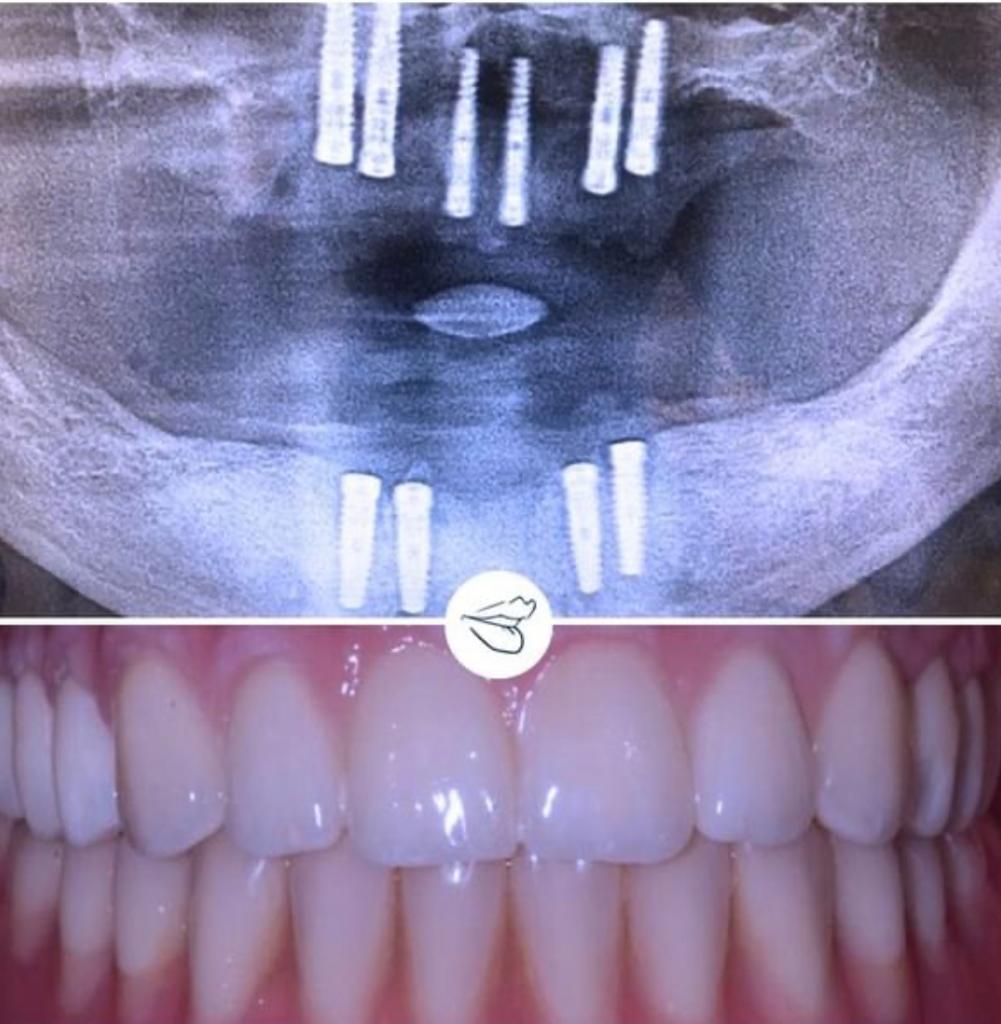
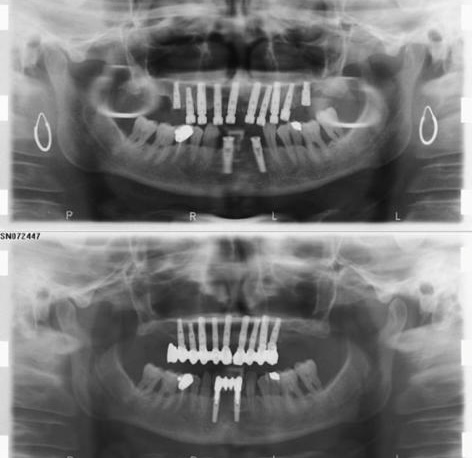
The implants must be anchored to the maxillary or mandibular bone just like natural teeth. If the patient bone volume is insufficient, it is still possible to turn to implantology because of bone augmentation techniques, after having carefully checked the patient’s health and diagnostic delay, which is fundamental for the underestimation of the problem.
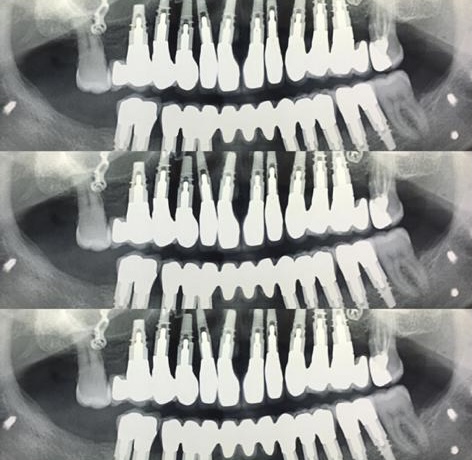
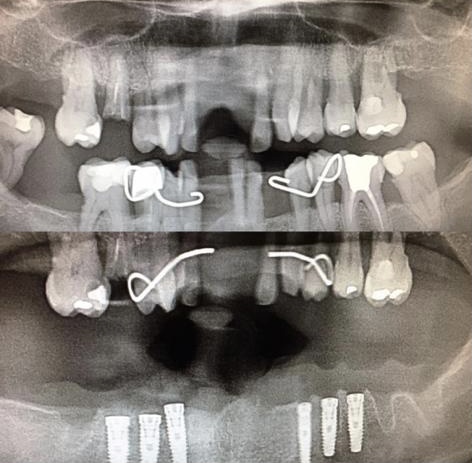
There are different bone regeneration techniques, aimed at inserting implants, in connection with the needs of individual patient.
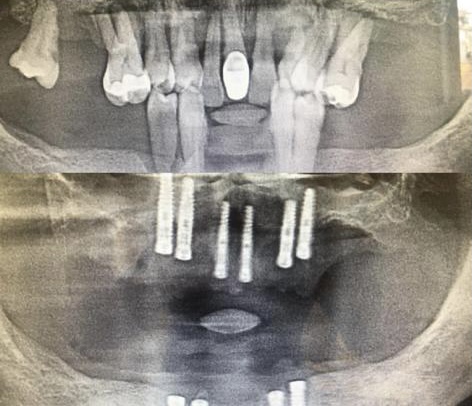
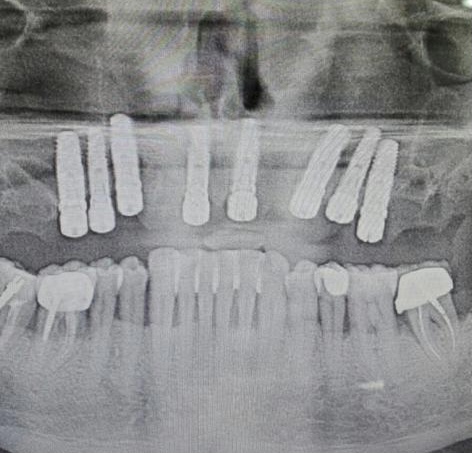
- Sinus lift / bone augmentation : this is a surgical procedure used to increase the height of the maxillary sinus, i.e. the air-filled bone cavity generally located in the upper part of the premolars and molars roots. This method involves lifting the mucosa lining the sinus cavity and grafting a replacement of natural or artificial material, which will form the new bone tissue, together with possible contextual integration of dental implants.
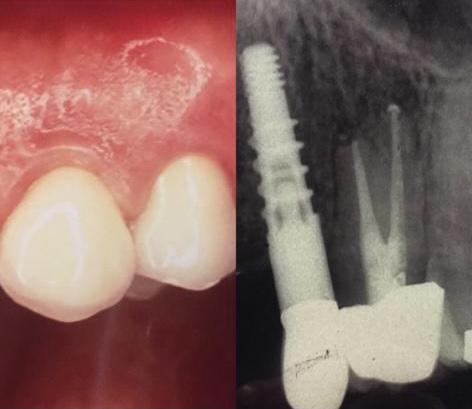
- Guided bone regeneration: this regenerative technique involves the use of a re-absorbable membrane, such as a collagen membrane, or a non-resorbable one, such as titanium grids, in order not to allow the gingival tissue to migrate inside the cavity, where instead the bone will have to be inserted, which can be either the patient’s own or dental supplying bank or of animal / synthetic origin. Implants can be inserted at the same time also in this case.
- Preservation of the implant within the hole left free by the tooth.
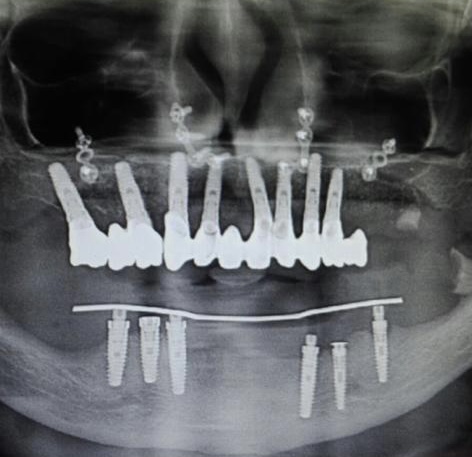
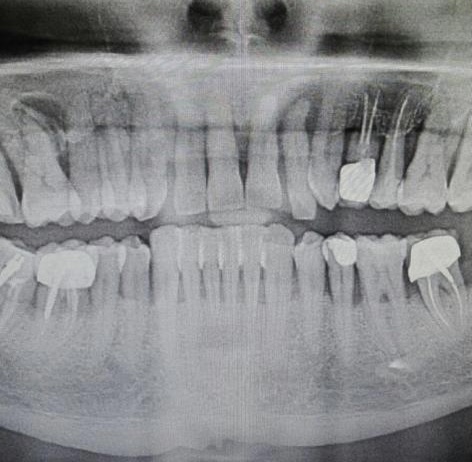
A careful assessment must be dedicated to osteoporotic patients. For patients being treated with anti-osteoporosis drugs, the interdisciplinary collaboration between dentistry and medical internist and / or endocrinologist and / or rheumatologist can be of great advantage, in order to have an integrated management of the patient, so as to bring him to implant surgery in the best possible clonic conditions on one side and to decrease the percentage of implant failure avoiding possible osteonecrosis.
In case of osteoporosis – With the increasing aging of the population, dentistry increasingly intercepts patients in advanced or senile age, with a high prevalence of chronic pathologies and often in polypharmacological therapy. A particular category of patients is represented by people suffering from osteoporosis being treated with drugs such as bisphosphonates, for which there is evidence in the literature about a possible causal interaction between drug therapy and the early onset of jaw bones osteonecrosis, a kind of osteomyelitis linked to an actinomycetes infection.
For patients under bisphosphonate oral treatment, the
medicine should be discontinued at least two months
before the implant surgery; for those who take the drug
intravenously, the suspension must be at least one year
before. No contraindications to surgical procedures for
those who take other drugs.
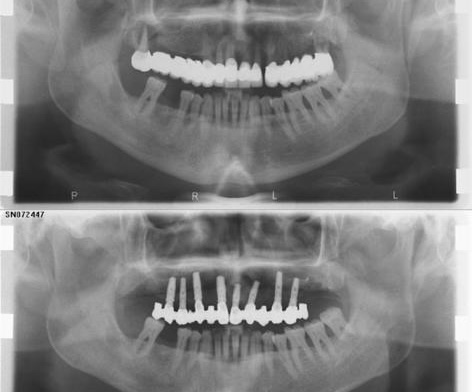
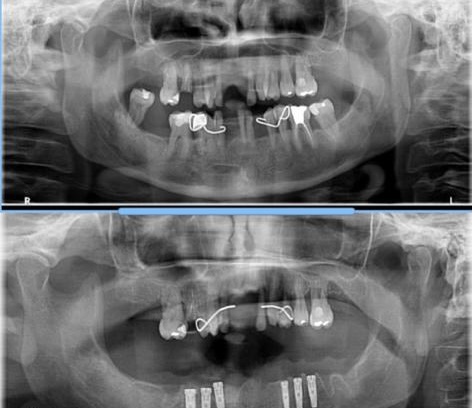
A minimally invasive surgery – The rehabilitations on a
limited number of implants have now been cleared by the
international literature. In daily clinical practice they can
be a suitable alternative to many cases in which the
patient’s conditions require a minimally invasive approach,
combining the reduced number of implants with a flapless
insertion, therefore without cuts and stitches. Just think of
all those patients, generally elder people, who are very
often associated with bone deficiency, even severe, to the
usually very critical clinical situation.